Why North Korea Is Buying More Insulin Than Ever
 Diabetes mellitus is a noncommunicable disease (NCD) that affects an estimated one to five million people in North Korea (Lin et al. 2020). Data regarding insulin supply, including data from Chinese customs, is useful, but limited. According to this customs data, North Korea has recently been importing unprecedently large amounts of insulin. Regardless of what this signifies, this momentum could present an opportunity for the international community and the Democratic People’s Republic of Korea (DPRK) to work together to address the needs of North Koreans living with diabetes and other NCDs.
Diabetes mellitus is a noncommunicable disease (NCD) that affects an estimated one to five million people in North Korea (Lin et al. 2020). Data regarding insulin supply, including data from Chinese customs, is useful, but limited. According to this customs data, North Korea has recently been importing unprecedently large amounts of insulin. Regardless of what this signifies, this momentum could present an opportunity for the international community and the Democratic People’s Republic of Korea (DPRK) to work together to address the needs of North Koreans living with diabetes and other NCDs.
Diabetes in North Korea
The prevalence of noncommunicable diseases is increasing in developing countries, and North Korea is no exception. The 2018 World Health Organization (WHO) NCD Country Profiles report estimated that NCDs account for 84 percent of all deaths in the DPRK, compared to the estimated 4.8 percent caused by communicable diseases (Ha and Lee 2019). The Global Burden of Diseases, Injuries, and Risk Factors Study found that for at least the past decade, the top three causes of death in the DPRK were stroke, ischemic heart disease and chronic obstructive pulmonary disease (COPD), all of which are NCDs.
The DPRK government has prioritized the prevention of NCDs as exemplified by their National Strategic Plan for the Prevention and Control of Noncommunicable Diseases in DPR Korea 2014-2020 (2014) and ratification of the WHO Framework Convention on Tobacco Control in 2005 (Hyon, 2017). NCDs are also included in the DPRK’s annual National Health Priority (NHP) plans and Medium Term Strategic Plan for Development of Health Sector DPRK (MTSP, 2016-2020) (Shin 2019; Hyon 2017). However, diabetes—another NCD—remains a significant hurdle for the country.
There are an estimated one to five million people living with diabetes mellitus (all types) in the DPRK (Lin et al. 2020), with approximately 0.8 million with Type 2 diabetes mellitus (T2DM) (Basu et al. 2019). If left untreated, T2DM can lead to devastating complications such as chronic kidney disease, blindness, limb amputations and death. It can be treated with oral medications and/or insulin injections, and makes up one percent of all NCD-related deaths in DPRK (2018 WHO NCD report).
Over the years, North Korea has devoted more attention and resources to drugs for chronic diseases—such as cardiovascular disease and diabetes mellitus at the household level (Hyon 2017)—and recently reported that half of the essential NCD medicines and technologies were generally available within the country.
Chinese Customs Data[1]
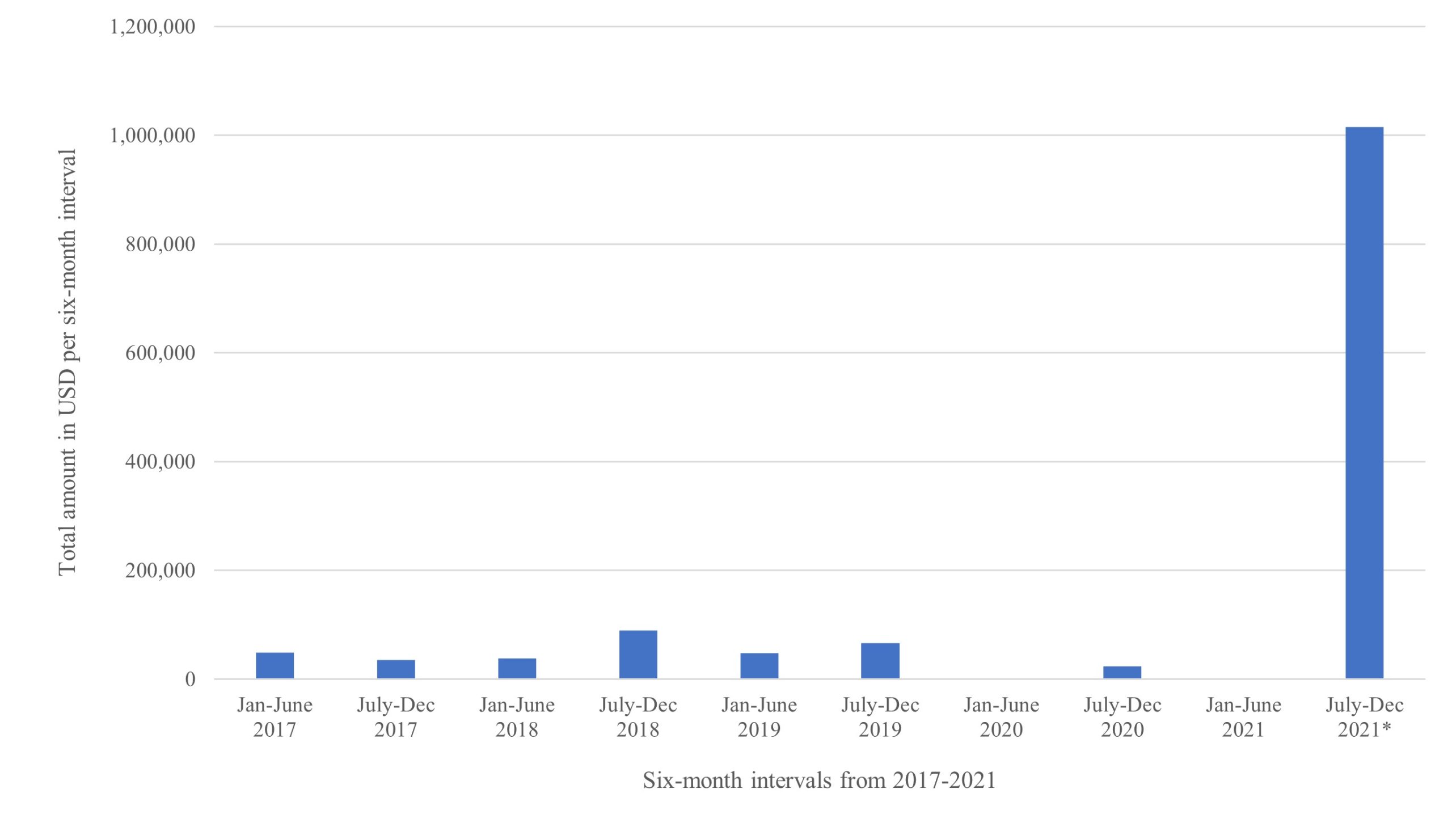
To further investigate the treatment of NCDs in the DPRK, the Harvard Korea Health Project team analyzed insulin imports into the DPRK from China as a surrogate estimator for diabetes treatment coverage. We used publicly available monthly Chinese export data to the DPRK dating back to 2017. We found that the pre-pandemic six-month average total insulin import (in USD) was $54,322.17. According to summarized customs data, the major drop in trade due to COVID-19 virus border closures occurred in February 2020. The six-month average insulin import during the pandemic border closure (from February 2020 to June 2021) was $7,733.33, meaning that insulin imports dropped by 85.8 percent. However, for the first time in a year, there was a massive import of insulin in July 2021, totaling $409,500.00, and then again in November 2021, totaling $605,658.00.
Figure 1. Total insulin imports (in USD) into DPRK from China divided into six-month intervals.
Calculation of the Number of People with Insulin-Dependent Type 2 Diabetes Mellitus That Reported Insulin Imports Could Treat[2]
There are an estimated 822,711 people living with type 2 diabetes mellitus in the DPRK (Basu et al. 2019).
According to the Korea National Health and Nutrition Examination Survey, three percent of South Koreans with type 2 diabetes are insulin dependent. However, other studies such as the Joint Asia Diabetes Evaluation Registry as well as similar studies in China and the Philippines have shown 14.4 percent, 18.3 percent, and seven percent, respectively. Averaging the insulin dependence rates across these studies yields 11.2 percent. While likely on the higher side, applying this rate in the case of DPRK would mean an estimated 92,144 North Koreans are living with insulin-dependent type 2 diabetes (ID-T2DM).
It is estimated that in Asia, the total number of insulin U100 vials (each containing 10 milliliters (mL), or 1,000 units) used per year is 577,108,650 (Basu et al. 2019). If we take this total and divide it by the number of people in Asia living with ID-T2DM (37,619,272 people), we find that each person with ID-T2DM uses on average 15.34 vials per year, or 7.67 vials every six months.
Unfortunately, the Chinese customs data only reports total kilograms (kg) and cost of insulin imported, not the number of vials, units or specific types and concentrations of insulin. As such, we must make the broad assumption that a U100 insulin vial[3] most likely weighs around 40 grams (with the glass casing). Before the pandemic border closure, the six-month average total kg insulin import was 1,322 kg. This means that an average of 33,050 vials (an estimated 1,322 kg/0.04 kg per vial) were imported every six months. After the border closure, the six-month average was 250 kg, translating to an average of 6,250 vials imported every six months. The DPRK began allowing limited imports again around July 2021 including 4,780 kg of insulin in July 2021, and 6,444 kg in November 2021. These two shipments represent the largest bulk insulin imports by far, at least since 2017. Using our assumption again of 0.04 kg per vial, these recent shipments included approximately 280,600 vials (11,224 kg/0.04 kg per vial).
For type 2 insulin-dependent diabetics, this means:
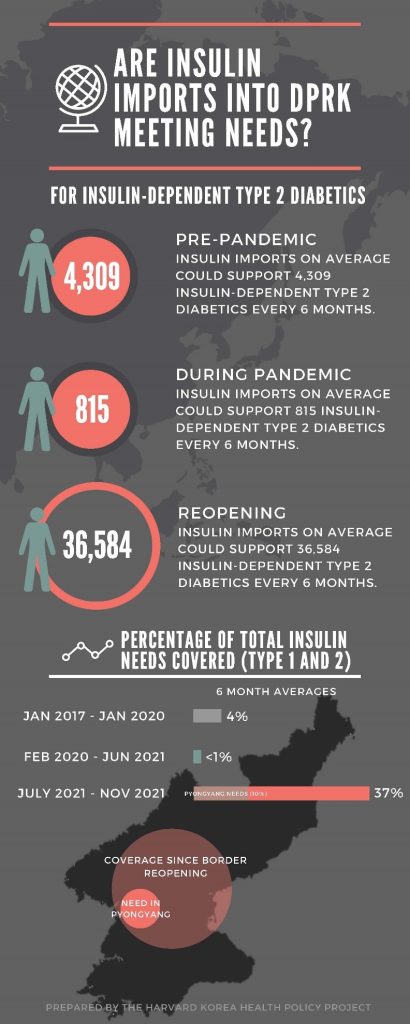
At 7.67 vials per person every six months, the pre-pandemic six-month average could support 33,050 vials/7.67 vials per person = 4,309 people every six months, whereas it could support only 6,250 vials/7.67 vials per person = 815 people per six months during the pandemic border closure. Post-closure imports could support 280,600 vials/7.67 vials per person = 36,584 people every six months.
Calculation of the Number of People with Insulin-Dependent Type 1 Diabetes Mellitus That Reported Insulin Imports Could Treat
It is estimated that the prevalence of T1DM is 0.017-0.021 percent in South Korea (Song 2016). Given that Type 1 diabetes is an autoimmune disease based more on genetics rather than behavioral or environmental factors, it is reasonable to use this estimate for North Korea’s population. Using the middle of that range (0.019 percent) and assuming an estimated population of 25 million people in North Korea, there are likely around 4,750 people with type 1 diabetes in North Korea.
We will assume that an average type 1 diabetic needs about one unit/kg/day of insulin (a conservative estimate that is likely overestimating the insulin needs, as adolescent and adult patients typically are started on 0.6-0.7 units/kg/day). Needs vary depending on age and weight, which can be hard to determine given the lack of hard data available. In South Korea, the reported median age of entry into the type 1 diabetes registry is 37.1 years old; however, the highest proportion of new entries are in the 15-19 years age group (Song 2016). Given that children weigh less and thus require less insulin, we will use 50 kg as the average type 1 diabetic weight. At one unit/kg/day, this would be 50 units per day. With 1,000 units per vial, this would be about one vial every 20 days, or nine vials every six months.
Just looking at the type 1 diabetic population, before the pandemic border closure, insulin imports could support 3,672 type 1 diabetics (33,050 vials/nine vials per person) for six months. After the shutdown, this would drop to 694 type 1 diabetics (6,250 vials/nine vials per person) covered every six months. The post-closure insulin imports (since July 2021) could support 31,178 type 1 diabetics (280,600 vials/nine vials per person) for six months.
Overall Insulin Needs (Type 1 and Type 2)
Looking at overall needs for all people in the DPRK needing insulin (including insulin-dependent type 2 diabetics and type 1 diabetics), North Korea would need to import around 749,494 vials every six months (see calculations below). It was meeting 4.4 percent of this need prior to the pandemic border closure, 0.8 percent of this need during the border closure (from February 2020 to June 2021), and 37.4 percent since July 2021.
Type 2 insulin-dependent diabetics: 7.67 vials * 92,144 people = 706,744 vials every six months.
Type 1 diabetics: Nine vials * 4,750 people = 42,750 vials every six months.
This is a total of 749,494 vials every six months.
Figure 2. Are Insulin Imports Into DPRK Meeting Needs?
Discussion
From these calculations, we find that there is a significant unmet burden of diabetes mellitus treatment in the DPRK, with imports of insulin even before the pandemic covering only a small percentage (4.4 percent) of the insulin needed to meet the demand of its people living with insulin-dependent diabetes. The overall trend of insulin imports was upward before the pandemic. Then with the pandemic era border closures, almost no insulin was being imported from China. However, since July 2021, there have been large rebound shipments that could cover approximately 37 percent of the total nationwide insulin need. Assuming that Pyongyang makes up at least 10 percent of total insulin needs given its population size, these recent imports can cover almost four times the amount of insulin needed to treat all insulin-dependent diabetic patients (types 1 and 2) in Pyongyang. This could reflect North Korea’s commitment to treating diabetes, even outside of the elites of Pyongyang, and/or that their stocks were running critically low during the pandemic shutdown. It is unlikely that the diabetes population acutely surged, so these recent large imports could signify the Ministry of Public Health’s prioritization of diabetes diagnosis and treatment within the country. Two relatively massive shipments within a few months of each other suggest consumption and not stockpiling of medicine, especially given the storage limitations (see below).
It is essential to consider a few additional factors.
- First, the shelf life of insulin is 28 days unrefrigerated. If refrigerated, the shelf life is about one year until opened. Once opened, the shelf life is 28 days. Taking their vaccine cold chain capabilities as an example, North Korea should have the ability to handle the storage and distribution of insulin (Shafik 2021). However, it is unknown if and how insulin is being distributed.
- Second, many of the 92,144 estimated insulin-dependent type 2 diabetic and 4,750 type 1 diabetic populations are likely to be undiagnosed, highlighting the importance of increasing diagnostic capabilities throughout rural areas in North Korea and extending projects like Package of Essential NCD interventions outside of Pyongyang.
- Third, insulin and oral diabetes drugs could potentially be fabricated by PyongSu Pharma, although it is unlikely to be operating at full capacity given the lack of raw materials and laboratory reagents due to the sanctions.
- Fourth, insulin alone is not enough. Treatment of diabetes also necessitates glucometers, glucose strips, hypoglycemia kits, syringes, oral diabetic medications, etc.
- Fifth, it is unclear if this Chinese customs data reflects direct buys from the North Korean government or NGOs and international agencies importing into the country. Most likely, it represents a combination of both. For example, according to the United Nations Panel of Experts Report S/2021/211 pg. 393, several batches of humanitarian goods were still being imported through China into DPRK from January to October 2020, although only a fraction of what was being imported before, and it is unclear if the goods actually made it through the quarantine process. It is unlikely that all of these humanitarian batch shipments were reflected in the customs data. Furthermore, one NGO that independently ships insulin into the DPRK has confirmed their shipments were not reflected in the trade data. Therefore, Chinese customs data most likely underestimates the amount of insulin coming into the country. However, it is important to note that a very small minority of humanitarian organizations working in the DPRK focus on NCDs like diabetes mellitus.
- Sixth, there are multiple DPRK-specific and globally recognized barriers to maintaining insulin supply. International pressure against the DPRK has limited the amount of humanitarian aid coming into the country via mechanisms such as declining funding, increased burden of securing humanitarian exemption approvals, lack of a banking channel, and shipping difficulties and delays due to red tape. A recent WHO report demonstrated the massive disparities of insulin access in LMICs due to a variety of factors, including barriers with intellectual property rights and regulatory challenges, pricing and affordability, supply and distribution chain management, market structure, interchangeability of insulins, lack of affordable supportive devices, and local health system factors.
Conclusion
Diabetes mellitus prevalence will continue to increase, with estimates at 944,538 people with type 2 DM by 2030 in the DPRK (Basu et al. 2019). The DPRK seems to have recognized and prioritized diabetes treatment recently, evidenced by their relatively massive imports of insulin since July 2021, the monetary value of which was 11 times larger than any six-month period before the pandemic border closure since 2017. As North Korea reopens its borders, analyzing insulin imports may inform researchers of trends on investment and health prioritization. However, many challenges to ensuring adequate insulin coverage in the DPRK remain. Broadly, these include sanction-induced barriers for the DPRK to manufacture insulin and antidiabetic medications, general lack of funding for NCDs by international humanitarian organizations (WHO being one of the only major organizations that works on NCDs in the DPRK), and the pricing and feasibility issues for securing insulin in LMICs as laid out in the WHO report. However, this report also proposed pathways that the international community and countries can take to improve access to insulin. This is an opportunity for the international community and the DPRK to work together to address the growing needs of North Koreans living with diabetes mellitus and other NCDs.
References
Basu Sanjay, Yudkin JS, Kehlenbrink S, Davies JI, Wild SH, Lipska KJ, Sussman JB, Beran D. “Estimation of global insulin use for type 2 diabetes, 2018-30: a microsimulation analysis.” Lancet Diabetes Endocrinol 7, no. 1 (January 2019): 25-33. https://doi.org/10.1016/s2213-8587(18)30303-6.
Ha Shin, Lee YH. “Underestimated Burden: Non-Communicable Diseases in North Korea.” Yonsei Med J 60, no. 5 (May 2019): 481-483. https://doi.org/10.3349/ymj.2019.60.5.481.
Hyon Choe Suk, Nam KY, Sun HC, Garg R, Shrestha SM, Ok KU, Kumar R. “Package of essential noncommunicable disease (PEN) interventions in primary health-care settings in the Democratic People’s Republic of Korea: A feasibility study.” WHO South East Asia J Public Health 6, no.2 (September 2017): 69-73. https://doi.org/10.4103/2224-3151.213794.
Lin Xiling, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. “Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025.” Sci Rep 10, no. 1 (September 2020):14790. https://doi.org/10.1038/s41598-020-71908-9.
Song Sun Ok, Song YD, Nam JY, et al. “Epidemiology of Type 1 Diabetes Mellitus in Korea through an Investigation of the National Registration Project of Type 1 Diabetes for the Reimbursement of Glucometer Strips with Additional Analyses Using Claims Data.” Diabetes Metab J 40, no. 1 (February 2016): 35-45. https://doi.org/10.4093/dmj.2016.40.1.35.
Shafik Nagi M., Ryder CY, Park KB. “North Korea’s Vaccination Capabilities: Implications for a COVID-19 Campaign.” 38 North. August 5, 2021. https://www.38north.org/2021/08/north-koreas-vaccination-capabilities-implications-for-a-covid-19-campaign/.
Shin Bo Kyung, Jeon WT. “National Health Priorities under the Kim Jong Un regime in Democratic People’s Republic of Korea (DPRK) 2012–2018.” BMJ Global Health, no. 4 (Supple 7) (2019): e001518. https://dx.doi.org/10.1136%2Fbmjgh-2019-001518.
- [1]
There are certain drawbacks to using Chinese customs data. There is a lack of clarity whether the Chinese customs data represents all of the items coming into the country. Some commodity codes are vague. It also does not include any trade at other sites like the Pyongyang airport, which has been closed since the pandemic but may have accepted humanitarian goods before then. See discussion section for more details.
- [2]
Given the sparsity of data, please note these are rough calculations and are intended to give only our best estimate.
- [3]
There are various types of insulin that have different packaging and weights. Here we are assuming North Korea is shipping in U100 insulin vials, which can contain either short-acting or long-acting insulin. We based our weight calculation on the estimated weight of a glass vial of 10 mL of U100 insulin; however, this could be inaccurate.